Frequently Asked Questions About LVAD
What is an LVAD or MCS?
What is an LVAD or MCS?
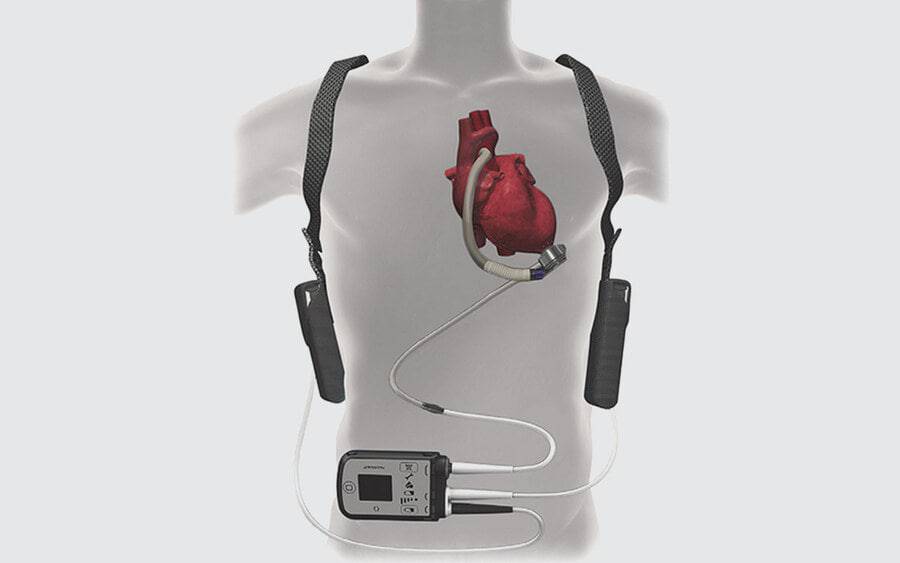
A ventricular assist device (VAD) is a blood pump that improves blood flow through the body. These devices do not replace the heart, but they do help it pump blood to the vital organs of the body, such as the kidney, brain and liver.
Many types of heart pumps are available, but the pumps that are FDA-approved for long-term use are commonly referred to as “left ventricular assist devices” (LVADs), because the pump is surgically implanted in the left ventricle of the heart. Patients must undergo cardiothoracic surgery to implant the devices.
Scripps heart failure specialists are committed to using the most advanced technology to treat heart failure and heart disease.
Find answers to common questions below, and visit our LVAD section to learn more.
What does LVAD stand for?
LVAD stands for left ventricular assist device. It is a type of mechanical circulatory support (MCS), often called a pump. It works by pumping oxygen-rich blood from the heart to the body.
When is LVAD needed?
Heart failure is a complex condition in which the heart muscle can no longer pump sufficient blood and oxygen to vital organs of the body.
An LVAD helps improve the hemodynamic (blood flow) function and boost cardiac output.
When medications are no longer enough to support the heart and the patient has end-stage heart failure an LVAD may be considered. For patients waiting for a heart transplant, an LVAD may help them survive until a donor heart is found. Not all patients are candidates for a heart transplant due to other preexisting conditions or their age. These patients may benefit from long-term VAD support.
Is the LVAD an artificial heart?
No. LVAD works with your heart, but it does not replace it.
Is the LVAD a pacemaker?
No. LVAD does not deliver electrical impulses to your heart muscles. Patients typically keep their pacemaker/defibrillator even with an LVAD.
What are the risks and possible complications associated with LVADs?
Complications of LVAD surgery are similar to the potential complications of any open heart surgery. Some of the possible complications related to the LVAD include bleeding, infection, device malfunction, right heart failure, kidney failure, stroke and pump clot or death. Your surgeon will discuss the benefits and potential risks in detail with you prior to the procedure.
What can I expect in terms of quality of life and what improvements will I see after I get an LVAD?
Our goal is to get you back to living as normal a life as possible. While there are some restrictions, the majority of patients experience a significant increase in their quality of life after the LVAD is implanted.
How long does LVAD implant surgery take?
Surgery to implant an LVAD usually takes from four to six hours.
How soon can I expect to go home with the LVAD?
The average length of hospital stay for LVAD patients is two to three weeks. Care is individualized to meet patient needs.
How long is LVAD recovery time?
After LVAD surgery, most patients generally spend three to five days recovering in the ICU at Prebys Cardiovascular Institute, and then move to a regular hospital room. Most patients are in the hospital for 2-3 weeks.
During this time, our physical and occupational therapists and dietitians will work with you to speed up your recovery process. We will continue to educate you and your care partner about caring for the LVAD, and your care partner will participate in driveline dressing changes with the LVAD coordinator.
Following your hospital stay, you will either go home or to an inpatient rehabilitation program, depending on your strength and overall needs. At the rehab facility, we focus on helping you build your strength and prepare to go home. You and your care partner will also have the chance to finish up any education about LVAD care and driveline dressing changes.
What about rehabilitation after LVAD surgery?
Some patients will go to inpatient cardiac rehabilitation after their LVAD is implanted, while others are discharged directly home with home-based physical therapy and occupational therapy visits.
What kind of help will I need after my surgery?
You will need a care partner with you 24 hours a day for at least two to three weeks after LVAD implantation. Once you get stronger, the LVAD team will discuss increasing your independence. Each patient will receive a detailed, personalized post-surgery care plan. Your caregiver will discuss with you how to recognize the first signs of complication so problems can be treated as quickly as possible.
Why do I need a caregiver?
Your caregiver will help take care of you while you are recovering from surgery. They will also be trained on the LVAD equipment so they can recognize alarms and know how to respond. You will need help getting to and from clinic appointments while you are recovering. Your caregiver will also be responsible for doing the lifelong dressing changes where the tube comes out of your abdomen.
Can I shower after receiving an LVAD?
Showering is dependent on when your LVAD driveline exit site is healed. Your LVAD coordinator will advise you when it is safe to shower.
What activities are prohibited after I’ve had LVAD surgery?
Driving is restricted until your breastbone (sternum) heals. We will discuss this with you on your follow-up visits. Totally restricted activities include swimming (equipment and driveline cannot be submerged in water), contact sports and arc welding. Women are not to become pregnant while on LVAD support because of device-related complications.
Will I be able to have sex after I have an LVAD?
Yes, however your breastbone will need to be completely healed. You must be able to walk up two flights of stairs without becoming overly tired before sexual relations are allowed. Please discuss your recovery status with your physician before engaging in sexual activity.
Will I be able to work after my surgery?
Yes, depending on the kind of work you do you should be able to return to work once you’ve recovered from surgery. Please discuss this with your LVAD team.
What happens if my LVAD malfunctions?
We will provide you with education on what to do during these situations, as well as a phone number for access to the LVAD team 24 hours a day, seven days a week in the event of an emergency.
How long does the LVAD last?
The Food and Drug Administration (FDA) has approved LVADs for use for five years. However, lab tests suggest that it could last 15 years to 20 years because there is minimal to no wear on the pump itself.
How long do the LVAD batteries last?
According to the manufacturers, a set of fully charged batteries will last from 16-18 hours. The actual battery life depends on the amount of power required to run the pump. LVAD batteries are recharged nightly when plugged into a power module.
Is it normal to not feel a pulse after getting the LVAD?
Yes. Your pump has what’s called continuous flow. Because of this, patients may or may not have a pulse, so it is normal if you don’t feel one.
How much do LVADs weigh?
The device itself weighs almost 1 pound, and the equipment that you wear daily weighs around 4 pounds combined.
Will I be on blood thinners?
Yes, patients are on both Warfarin and aspirin. There are rare exceptions to this. Your care team will discuss all of your medications with you and any side effects that you may experience from blood thinners.
Can LVAD be removed?
Yes, an LVAD can be removed once the heart regains strength and can support the body’s needs, but this is very rare <5%).
Can an LVAD be replaced?
When certain complications occur it may be necessary to replace the pump.
Can LVAD patients have an MRI?
No, patients may not have MRIs.
Can LVAD patients travel?
Yes, LVAD patients can travel! You get an LVAD to improve your quality of life and that includes traveling. Your LVAD coordinators work with you to provide letters and instructions for safe travel. They will inform the LVAD center nearest to where you are traveling that you are in the area in case you need emergency care.
What is LVAD driveline?
A thin cord called a driveline runs from the LVAD motor through a tiny opening in the skin and connects to the controller and batteries outside the patient’s body. Your caregiver learns to put a sterile dressing over this site.