Scripps Health | Hospitals and Clinics in San Diego

Here for You.
Here for Good.
We’re here for you with exceptional health care and leading-edge facilities — all focused on your needs. With a network of physicians and specialists at 30 locations throughout San Diego County, we offer comprehensive, personalized care for your health and wellness.

Innovating Care, Elevating Experience
Welcome to the next era of health care at Scripps Memorial Hospital La Jolla. Opening June 2025, the new North Tower features state-of-the-art imaging and advanced technology, ensuring people throughout San Diego receive leading-edge care now and for years to come.

Virtual Care
Get the care you need this spring with our convenient telemedicine options. Whether its allergies, asthma, sinus infections or other health concerns, you can quickly connect with a Scripps doctor or nurse practitioner through a live video visit.
News and Articles
View our latest news, videos and health tips

New $664M North Tower Opens at Scripps Memorial Hospital La Jolla
The new North Tower at Scripps Memorial Hospital La Jolla features comprehensive mother-baby services and advanced technology operating rooms.

ABC 10 News Shares Inspiring Cancer Survivors Day Story
After advanced breast cancer treatment at Scripps, Michelle Fernandez is thriving. ABC 10 News explores her inspiring Cancer Survivors Day story.

What Are Cancer Screenings Men Should Not Ignore?
Men should not ignore or delay cancer screenings, especially for prostate and colon cancers. Early detection saves lives.

Pap Test vs HPV Test: What’s the Difference?
A Pap test and an HPV test are both effective screenings for cervical cancer, but they look for different things. Early detection saves lives.

Media Get ‘Sneak-Peek’ Inside New Hospital Tower
Media outlets recently toured the North Tower on the campus of Scripps Memorial Hospital La Jolla, which opens on June 1.
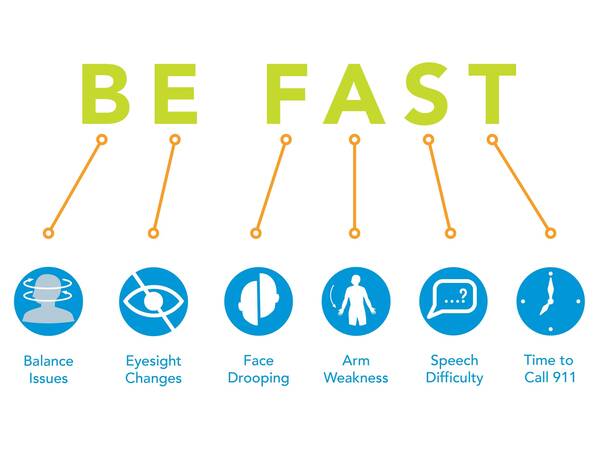
Act Fast to Stop a Stroke
Every year 800,000 people suffer a stroke in the US. Learn the warning signs for stroke symptoms. Learn the acronym BE FAST.





